Test your blood pressure IQ using our new infographic! How many facts about blood pressure did you already know?

Category Archives: Heart Disease
Hypercortisolism Is Associated With Increased Coronary Arterial Atherosclerosis
Hypercortisolism Is Associated With Increased Coronary Arterial Atherosclerosis: Analysis of Noninvasive Coronary Angiography Using Multidetector Computerized Tomography
Journal of Clinical Endocrinology and Metabolism, 05/21/2013 Clinical Article
- Nicola M. Neary*,
- O. Julian Booker*,
- Brent S. Abel,
- Jatin R. Matta,
- Nancy Muldoon,
- Ninet Sinaii,
- Roderic I. Pettigrew,
- Lynnette K. Nieman and
- Ahmed M. Gharib
–Author Affiliations
Program in Reproductive and Adult Endocrinology (N.M.N., L.K.N., B.S.A.), Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland 20892; Laboratory of Cardiac Energetics (O.J.B.), National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Maryland 20892; Integrative Cardiovascular Imaging Laboratory (J.R.M., R.I.P., A.M.G.), National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland 20892; Critical Care Medicine (N.M.), Clinical Center, National Institutes of Health, Bethesda, Maryland 20892; and Biostatistics and Clinical Epidemiology Service (N.S.), Clinical Center, National Institutes of Health, Bethesda, Maryland 20892
- Address all correspondence and requests for reprints to: Ahmed M. Gharib, MB, ChB, National Institutes of Health, Building 10, Room 3-5340, Mail Stop Code 1263, 10 Center Drive, Bethesda, MD 20892. E-mail: agharib@mail.nih.gov.
-
↵* N.M.N. and O.J.B. contributed equally to this work.
Abstract
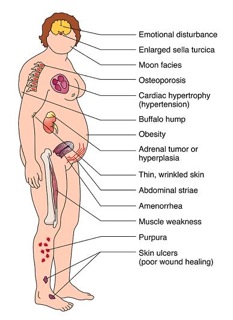
Background: Observational studies show that glucocorticoid therapy and the endogenous hypercortisolism of Cushing’s syndrome (CS) are associated with increased rates of cardiovascular morbidity and mortality. However, the causes of these findings remain largely unknown.
Objective: To determine whether CS patients have increased coronary atherosclerosis.
Design: A prospective case-control study was performed.
Setting: Subjects were evaulated in a clinical research center.
Subjects: Fifteen consecutive patients with ACTH-dependent CS, 14 due to an ectopic source and 1 due to pituitary Cushing’s disease were recruited. Eleven patients were studied when hypercortisolemic; 4 patients were eucortisolemic due to medication (3) or cyclic hypercortisolism (1). Fifteen control subjects with at least one risk factor for cardiac disease were matched 1:1 for age, sex, and body mass index.
Primary outcome variables: Agatston score a measure of calcified plaque and non-calcified coronary plaque volume were quantified using a multidetector CT (MDCT) coronary angiogram scan. Additional variables included fasting lipids, blood pressure, history of hypertension or diabetes, and 24-hour urine free cortisol excretion.
Results: CS patients had significantly greater noncalcified plaque volume and Agatston score (noncalcified plaque volume [mm3] median [interquartile ranges]: CS 49.5 [31.4, 102.5], controls 17.9 [2.6, 25.3], P < .001; Agatston score: CS 70.6 [0, 253.1], controls 0 [0, 7.6]; P < .05). CS patients had higher systolic and diastolic blood pressures than controls (systolic: CS 143 mm Hg [135, 173]; controls, 134 [123, 136], P < .02; diastolic CS: 86 [80, 99], controls, 76 [72, 84], P < .05).
Conclusions: Increased coronary calcifications and noncalcified coronary plaque volumes are present in patients with active or previous hypercortisolism. Increased atherosclerosis may contribute to the increased rates of cardiovascular morbidity and mortality in patients with glucocorticoid excess.
- Received October 29, 2012.
- Accepted March 7, 2013.
- Copyright © 2013 by The Endocrine Society
From JCEM
Related articles
- Cushing’s syndrome increased risk for coronary arterial atherosclerosis (maryomedical.com)
- Know Your Number (cushieblog.com)
- Coronary Artery Calcium Buildup Increases Heart Attack Risk (medindia.net)
Classifying hypertension
HYPERTENSION is classified into two categories according to its cause: essential and secondary.
The vast majority of patients have essential or primary hypertension, while only about 5-10% of patients have secondary hypertension, which are mainly caused by kidney and hormonal conditions like renal artery stenosis, hyperthyroidism, Cushing’s syndrome, and even pregnancy, among others.
The exact cause of essential hypertension is still unknown, although it is certainly the result of a combination of factors, including increasing age, having relatives with high blood pressure (ie family history), a sedentary lifestyle, a poor diet with too much salt, drinking too much alcohol, smoking and too much stress.
Says Malaysian Society of Hypertension president and Universiti Malaya Department of Primary Care Medicine senior consultant Prof Datin Dr Chia Yook Chin: “Each factor increases blood pressure by just a little, but when you add them all together little by little, it raises it by quite a lot.”
Despite not knowing the root cause of hypertension, it has been established that there is overstimulation of the sympathetic nerves in people with this condition.
This in turn increases the secretion of certain hormones involved in the regulation of sodium and fluids in the body, called renin, angiotensin, and aldosterone.
The amount of salt and water in our body affects our blood pressure – the more salt and water present, the higher our blood pressure.
These two elements are regulated by our kidneys through the three hormones mentioned above, which are produced by the adrenal glands located on top of the kidneys.
The overstimulation of the sympathetic nerves also results in increased vascular tone, which causes our arteries to become constricted, thus, also raising blood pressure.
From The Star
Related articles
- Hypertension, commonest cardiovascular disorder, says Cardiologist (vanguardngr.com)
- World hypertension day: Know your numbers (business.inquirer.net)
- If you have high blood pressure yoga just may help you (housewivesmag.wordpress.com)
Minimally Invasive Multivessel CABG
This is a video showing Coronary Artery Bypass Grafting being done through left 4th intercostal space by a 6-7cm incision.
We are routinely doing Coronary Artery Bypass Grafting, single vessel or multivessel through left 4th or 5th Intercostal Space depending on position of apex of heart and the target arteries on routine chest x-ray and coronary angiogram. We are using skeletonised LIMA and Free Radial Artery to construct a ‘Y’ and then pick all the vessels to be grafted sequentially. Single Lung ventilation using an endobronchial tube is essential.
Team Includes Dr.Kshitij Dubey (Chief Cardiac Surgeon), Dr. Vikas Gupta (Chief Cardiac Anaesthetist), Dr. Krishnpal Singh (Anaesthetist) Mr.M.V.Krishna Mohan (Sr.Clinical Perfusionist), Rajshree Hospital & Research Centre, Indore, Madhya Pradesh.
Related articles
- Heart attacks: What you should know (maryomedical.com)
- Effects of Off-Pump and On-Pump Coronary-Artery Bypass Grafting at 1 Year (maryomedical.com)
- News From The Annals Of Internal Medicine: April 23, 2013 (medicalnewstoday.com)
- At the heart of a keyhole revolution (telegraph.co.uk)
- CABG Surgery Generally Not Associated With Long-Term Cognitive Dysfunction (medicalnewstoday.com)
A heart disease infographic
Matters of Your Heart Infographic from the American Heart Association
Cushing’s syndrome increased risk for coronary arterial atherosclerosis
 Neary NM. J Clin Endocrinol Metab. 2013;doi:10.1210/jc.2012-3754.
Neary NM. J Clin Endocrinol Metab. 2013;doi:10.1210/jc.2012-3754.
In a recent study supported by the NIH, researchers determined that patients with Cushing’s syndrome have a greater risk for developing coronary arterial atherosclerosis, increasing their rate of cardiovascular morbidity. These findings were published in the Journal of Clinical Endocrinology & Metabolism.
The researchers conducted a prospective case-control study of 15 consecutive patients with adrenocorticotropic hormone (ACTH)-dependent Cushing’s syndrome who were matched with 15 controls (aged 32 to 66 years) with at least one risk factor for cardiac disease (ie, diabetes, hypertension, hyperlipidemia, family history of early-onset coronary artery disease and previous or current smoking).
Researchers used a multidetector CT (MDCT) coronary angiogram scan to measure calcified and noncalcified coronary plaque volume and Agatston scores. Additional variables included fasting lipids, BP, history of hypertension or diabetes and 24-hour urine free cortisol excretion.
According to data, patients with Cushing’s syndrome had significantly greater noncalcified plaque volume and Agatston scores compared with controls (noncalcified plaque volume median [interquartile ranges]: 49.5 vs. 17.9,P<.001; Agatston score: 70.6 vs. 0, P<.05).
Patients with Cushing’s syndrome also demonstrated higher systolic (143 mm Hg) and diastolic (86 mm Hg) BP compared with controls (systolic: 134 mm Hg, diastolic: 76 mm Hg).
The limitations of the study include the small cohort of patients and potential selection bias due to ectopic ACTH secretion. However, the researchers wrote that these findings demonstrate a significant difference between the two groups included in the study.
“Overall, the findings point to the possible causes of cardiovascular morbidity in patients treated with exogenous steroids and indicate the need for further studies of that population,” they wrote.
Disclosure: The researchers report no relevant financial disclosures.
~~~~~~~~~~~~~~
PERSPECTIVE
 Alice C. Levine
Alice C. Levine
- It has long been recognized that endogenous hypercortisolism (Cushing’s syndrome) and administration of supraphysiologic doses of glucocorticoids are associated with increased mortality, primarily due to cardiovascular disease. Excess glucocorticoids induce all of the features of the metabolic syndrome including obesity with central weight gain, hypertension, impaired glucose tolerance/diabetes mellitus and dyslipidemia, all of which increase cardiovascular risk. In this small but well-designed study, the authors attempt to determine whether excess glucocorticoids have a direct adverse effect on the coronary vasculature. Utilizing multidetector computerized tomographic (MDCT) coronary angiography, a validated noninvasive method of assessing calcified and noncalcified coronary plaques, they compared measurements of coronary plaques (Agatston score) in 15 patients with ACTH-dependent Cushing’s syndrome (CS) vs. 15 age-, sex- and body weight-matched controls with at least one risk factor for cardiac disease. They found significantly greater coronary calcifications and noncalcified coronary plaque volumes in patients with active or previous hypercortisolism.There are obvious limitations to the study; most notably the small sample size, the predominance of patients with CS due to ectopic ACTH (14/15) and significantly more hypertension in the CS vs. the control group. However, other than the HTN, the groups were well-matched and there was no statistical difference in the Framingham risk scores between groups. This is the first study to demonstrate direct effects of CS on coronary plaque burden.The findings, while unsurprising, underscore several important features of CS which endocrinologists need to consider. Firstly, as there were no statistical differences in plaque burden in patients with CS who were eucortisolemic (4/15) vs. those who were hypercortisolemic (11/15) at the time of study, the effects of CS on the coronary vasculature may persist even after biochemical cure. Many previous studies in larger cohorts have similarly demonstrated that the adverse effects of high glucocorticoids on cardiovascular, metabolic, psychiatric and neurocognitive function may be only partially reversible with disease remission. Secondly, even adjusting for all the confounding variables, hypercortisolism seems to be an independent risk factor for the development of coronary artery disease. The possible mechanisms underlying this observation are discussed and include increases in prothrombotic factors, circulating levels of vascular endothelial growth factor (VEGF) and angiogenesis. It is also plausible that cortisol increases atherosclerosis through the mineralocorticoid rather than the glucocorticoid receptor, suggesting the possibility of treating this particular deleterious effect of hypercortisolism with a mineralocorticoid-receptor blocker such as spironolactone.
Within the CS group, no significant correlations were observed between the coronary plaque volumes and the duration of CS or urinary free cortisol (UFC) either at presentation or at the time of MDCT. Although this lack of correlation may also be attributable to the small sample size, it is well known that the onset of Cushing’s syndrome is often insidious and it is impossible to pinpoint the exact duration of the abnormality in most patients. This study’s finding of direct, adverse and possibly irreversible effects of hypercortisolism on the coronary vasculature should make endocrinologists even more vigilant in diagnosing and treating the disease as early as possible in its course.
- Alice C. Levine, MD
- Professor of medicine, division of endocrinology, diabetes and bone diseases
Co-Director of The Adrenal Center
Icahn School of Medicine
Mount Sinai, New York, NY
- Disclosures: Levine reports no relevant financial disclosures.
From Healio.com
Related articles
- Cushing’s Help (cushie.info)
- Cushing’s Awareness Month: Living With Stripes (survivethejourney.blogspot.com)
- The real reason you’ve put on weight? 8 health problems which could stop you shedding the pounds (sacratomatovillepost.com)
- Obesity May Not Be A Symptom Of Polycystic Ovary Syndrome (medicalnewstoday.com)
Cardiac Rehabilitation Starts Today!
DH finally starts his cardiac rehab today, just over 8 weeks after his triple bypass.
Cardiac rehabilitation (rehab) teaches you how to be more active and make lifestyle changes that can lead to a stronger heart and better health. Cardiac rehab can help you feel better and reduce your risk of future heart problems.
In cardiac rehab, you work with a team of health professionals. Often the team includes a doctor, a nurse specialist, a dietitian, an exercise therapist, and a physical therapist. The team designs a program just for you, based on your health and goals. Then they give you support to help you succeed.
If you have had a heart attack, you may be afraid to exercise. Or if you have never exercised, you may not know how to get started. Your cardiac rehab team will help you start slowly and work up to a level that is good for your heart.
Many hospitals and rehab centers offer cardiac rehab programs. You may be part of a cardiac rehab group, but each person will follow his or her own plan.
Who should take part in cardiac rehab?
Doctors often prescribe cardiac rehab for people who have had a heart attack or bypass surgery. But people with many types of heart or blood vessel disease can benefit from cardiac rehab. Rehab might help you if you have:
- Heart failure.
- Peripheral artery disease (PAD).
- Had or plan to have a heart transplant.
- Had angioplasty to open a coronary artery.
- Had another type of heart surgery, such as valve replacement.
Often people are not given the chance to try cardiac rehab. Or they may start a program but drop out. This is especially true of women and older adults. And that’s not good news, because they can get the same benefits as younger people. If your doctor suggests cardiac rehab, stay with it so you can get the best results.
Medicare will pay for cardiac rehab for people with certain heart problems. Many insurance companies also provide coverage. Check with your insurance company or your hospital to see if you will be covered.
What happens in cardiac rehab?
In cardiac rehab, you will learn how to:
- Manage your heart disease and problems such as high blood pressure and high cholesterol.
- Exercise safely.
- Eat a heart-healthy diet.
- Quit smoking.
- Reduce stress and depression.
- Get back to work sooner and safely.
Exercise is a big part of cardiac rehab. So before you get started, you will have a full checkup, which may include tests such as an electrocardiogram (EKG or ECG) and a “stress test” (exercise electrocardiogram). These tests show how well your heart is working. They will help your team design an exercise program that is safe for you.
At first your rehab team will keep a close watch on how exercise affects your heart. As you get stronger, you will learn how to check your own heart rate when you exercise. By the end of rehab, you will be ready to continue an exercise program on your own.
What are the benefits of cardiac rehab?
Starting cardiac rehab after a heart attack can lower your chance of dying from heart disease and can help you stay out of the hospital. It may reduce your need for medicine.
Cardiac rehab may also help you to:
- Have better overall health.
- Lose weight or keep weight off.
- Feel less depressed and more hopeful.
- Have more energy and feel better about yourself.
Changing old habits is hard. But in cardiac rehab, you get the support of experts who can help you make new healthy habits. And meeting other people who are in cardiac rehab can help you know that you’re not alone.
Adapted from CardioSmart.org
Related articles
- Cardiac Rehabilitation (harley-petersen.blogspot.com)
- Lifestyle change at heart of cardiac rehab programs (blueridgenow.com)
- My Journey To Strength (drclintonb.wordpress.com)
Common Foods Loaded with Excess Sodium
Eating too many salty foods can create all sorts of health problems, including high blood pressure. But did you know a lot of common foods are packed with excess sodium? It’s not just the french fries and potato chips you need to be careful with.
That’s why the American Heart Association/American Stroke Association is increasing awareness of sodium and the “Salty Six” – common foods that may be loaded with excess sodium that can increase your risk for heart disease and stroke.
Sodium overload is a major health problem in the United States. The average American consumes about 3,400 milligrams of sodium a day – more than twice the 1,500 milligrams recommended by the American Heart Association/American Stroke Association. That’s in large part because of our food supply; more than 75 percent of our sodium consumption comes from processed and restaurant foods.
 Be sure to keep in mind that different brands and restaurant preparation of the same foods may have different sodium levels. The American Heart Association’s Heart-Check mark—whether in the grocery store or restaurant helps shoppers see through the clutter on grocery store shelves to find foods that help you build a heart-healthy diet.
Be sure to keep in mind that different brands and restaurant preparation of the same foods may have different sodium levels. The American Heart Association’s Heart-Check mark—whether in the grocery store or restaurant helps shoppers see through the clutter on grocery store shelves to find foods that help you build a heart-healthy diet.
Sodium doesn’t just affect your heart health, but your physical appearance as well. Excess sodium consumption may make your face feel puffy, give you bags under your eyes, increase swelling in your fingers and make your jeans look, and feel, tighter. In fact, from an American Heart Association/American Stroke Association consumer poll, 75 percent of respondents stated that their pants feeling too tight is their least favorite effect of bloating which may be associated with excess sodium consumption.
As you gear up for your next grocery store run or order from the menu, keep the Salty Six in mind. All you need to do to make a heart-healthy choice is to look for the Heart-Check mark. Another helpful tool is the Nutrition Facts label on the package and calorie labeling in restaurants, which together with the Heart-Check mark helps you make wise choices for the foods you and your family eat. Make the effort to choose products that contain less sodium. It’s worth it!
Here’s a quick look at the Salty Six, the top sources for sodium in today’s diet (download the infographic as a pdf)
Article from http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyDietGoals/Salty-Six_UCM_446090_Article.jsp
Related articles
- High Salt Consumption Tied to 2.3 Million Heart Deaths – Bloomberg (bloomberg.com)
- American Heart Association Report: Adults need to reduce sodium intake (charlotte.news14.com)
- Study links too much salt to 2.3M deaths each year (cbsnews.com)
Warning Signs of Heart Disease & Heart Attack

An example of a heart attack, which can occur after the use of a performance-enhancing drug. (Photo credit: Wikipedia)
Preventing Heart Disease and Heart Attack Educational Video. U.S. Department of Health and Human Services
National Institutes of Health; National Heart, Lung, and Blood Institute; Act in Time to Heart Attack Signs; Item #56-042N, September 2001;
The dramatic, moving stories of three heart attack survivors and their families illustrate the importance of heeding heart attack warning signs and seeking medical care quickly. They vividly convey how a real heart attack may differ from the stereotypical “movie heart attack” and how getting immediate treatment can save lives. The warm and sympathetic narration by an emergency department physician explains what a heart attack is, the treatments that can save lives if given quickly, why many heart attack victims delay seeking care, and how to make a heart attack survival plan. Useful for health fairs, medical waiting rooms, community groups, and home viewing.
Producer: National Institutes of Health; Keywords: hhs.gov; public_safety; Creative Commons license: Public Domain.
Heart Attack Warning Signs. A heart attack is a frightening event, and you probably don’t want to think about it. But, if you learn the signs of a heart attack and what steps to take, you can save a life–maybe your own. What are the signs of a heart attack? Many people think a heart attack is sudden and intense, like a “movie” heart attack, where a person clutches his or her chest and falls over. The truth is that many heart attacks start slowly, as a mild pain or discomfort. If you feel such a symptom, you may not be sure what’s wrong. Your symptoms may even come and go. Even those who have had a heart attack may not recognize their symptoms, because the next attack can have entirely different ones. Women may not think they’re at risk of having a heart attack–but they are.
Learn more about women and heart attack. It’s vital that everyone learn the warning signs of a heart attack. These are: Chest discomfort. Most heart attacks involve discomfort in the center of the chest that lasts for more than a few minutes, or goes away and comes back. The discomfort can feel like uncomfortable pressure, squeezing, fullness, or pain. Discomfort in other areas of the upper body. Can include pain or discomfort in one or both arms, the back, neck, jaw, or stomach. Shortness of breath. Often comes along with chest discomfort. But it also can occur before chest discomfort. Other symptoms. May include breaking out in a cold sweat, nausea, or light-headedness. Learn the signs–but also remember: Even if you’re not sure it’s a heart attack, you should still have it checked out. Fast action can save lives-maybe your own.
After you learn more about heart attack, try a brief quiz to see if you know what to do if you or someone else has warning signs. How do you survive a heart attack? Fast action is your best weapon against a heart attack. Why? Because clot-busting drugs and other artery-opening treatments can stop a heart attack in its tracks. They can prevent or limit damage to the heart–but they need to be given immediately after symptoms begin. The sooner they are started, the more good they will do–and the greater the chances are for survival and a full recovery. To be most effective, they need to be given ideally within 1 hour of the start of heart attack symptoms. You can reduce your risk of having a heart attack—even if you already have coronary heart disease (CHD) or have had a previous heart attack. The key is to take steps to prevent or control your heart disease risk factors.
Six Key Steps To Reduce Heart Attack Risk; Taking these steps will reduce your risk of having a heart attack: Stop smoking; Lower high blood pressure; Reduce high blood cholesterol; Aim for a healthy weight; Be physically active each day. Manage diabetes.
Related articles
- Heart Attack Warning Symptoms (maryomedical.com)
- How To Survive A Heart Attack (dahliafashion.wordpress.com)
- What We Don’t Talk About: Heart Health in Women (persephonemagazine.com)
- Heart Disease: It’s not just a “guy thing.” (espirational.com)
- Tired? It Could Be Your Heart (abcnews.go.com)
Effects of Off-Pump and On-Pump Coronary-Artery Bypass Grafting at 1 Year
From the New England Journal of Medicine
André Lamy, M.D., P.J. Devereaux, M.D., Ph.D., Prabhakaran Dorairaj, M.D., David P. Taggart, Ph.D., Shengshou Hu, M.D., Ernesto Paolasso, M.D., Zbynek Straka, M.D., Leopoldo S. Piegas, M.D., Ahmet Ruchan Akar, M.D., Anil R. Jain, M.D., Nicolas Noiseux, M.D., Chandrasekar Padmanabhan, M.D., Juan-Carlos Bahamondes, M.D., Richard J. Novick, M.D., Prashant Vaijyanath, M.D., Sukesh Kumar Reddy, M.D., Liang Tao, M.D., Pablo A. Olavegogeascoechea, M.D., Balram Airan, M.D., Toomas-Andres Sulling, M.D., Richard P. Whitlock, M.D., Yongning Ou, M.Sc., Janice Pogue, Ph.D., Susan Chrolavicius, B.A., and Salim Yusuf, D.Phil. for the CORONARY Investigators
March 11, 2013
DOI: 10.1056/NEJMoa1301228
Coronary-artery bypass grafting (CABG) reduces mortality among patients with extensive coronary artery disease.1 CABG is usually performed with the use of cardiopulmonary bypass (on-pump CABG). With this approach, perioperative mortality is about 2%, and myocardial infarction, stroke, or renal failure requiring dialysis develop in an additional 5 to 7% of patients. The technique of performing CABG on a beating heart (off-pump CABG) was developed to reduce perioperative complications, some of which may be related to the use of cardiopulmonary bypass and to the cross-clamping of the aorta associated with the on-pump CABG procedure, and to improve long-term outcomes.
Read the entire article here

An example of a heart attack, which can occur after the use of a performance-enhancing drug. (Photo credit: Wikipedia)
.
Related articles
- On-Pump Bypass Compared To Off-Pump Bypass: 30-Day Neurocognitive Differences Disappeared By One-Year Follow Up (medicalnewstoday.com)
- Coronary Artery Bypass Graft (CABG off-pump) (maryomedical.com)
- Study Finds Fewer Complications After Off-Pump Bypass Surgery Versus On-Pump For High-Risk Patients (medicalnewstoday.com)
- CABG leads to fewer MIs and repeat revascularization vs. stenting (2minutemedicine.com)




